Abstract
Tuberculosis (TB) poses significant health challenges globally, contributing significantly to illness and mortality. Approximately one-fourth of the world’s population is believed to carry the tuberculosis bacterium, with a 5–10% lifetime risk of developing active TB disease. Timely identification of TB and rapid detection of drug resistance are crucial in mitigating its global impact. Clinical, radiological, bacteriological, and molecular methods are used to screen and diagnose TB. Microscopy, culture, and immunological methods are commonly employed. Although microscopy has been used for approximately a century, it has limitations, necessitating its use and evaluation alongside other diagnostic techniques for a complete and accurate diagnosis. Bacterial culture in solid and liquid media is still the gold standard recommended by the World Health Organization (WHO) for the diagnosis of TB, as it enables the isolation of Mycobacterium tuberculosis (MTB) as well as the detection of drug resistance. In recent years, promising modern solutions have emerged that aim to overcome the limitations of culture and microscopic examination methods in molecular diagnostic testing. In routine laboratories in resource-wealthy countries, methods such as Mycobacterium Tuberculosis Drug Resistance Plus (MTBDRplus), loop-mediated isothermal amplification (LAMP), line probe assay (LPA), GeneXpert, and whole genome sequencing are increasingly being used to diagnose and characterize TB and determine anti-TB drug susceptibilities. Our goal is to explore and assess the evolution, advancements, and future prospects in TB diagnosis, focusing particularly on the current laboratory methods used for diagnosing the disease.
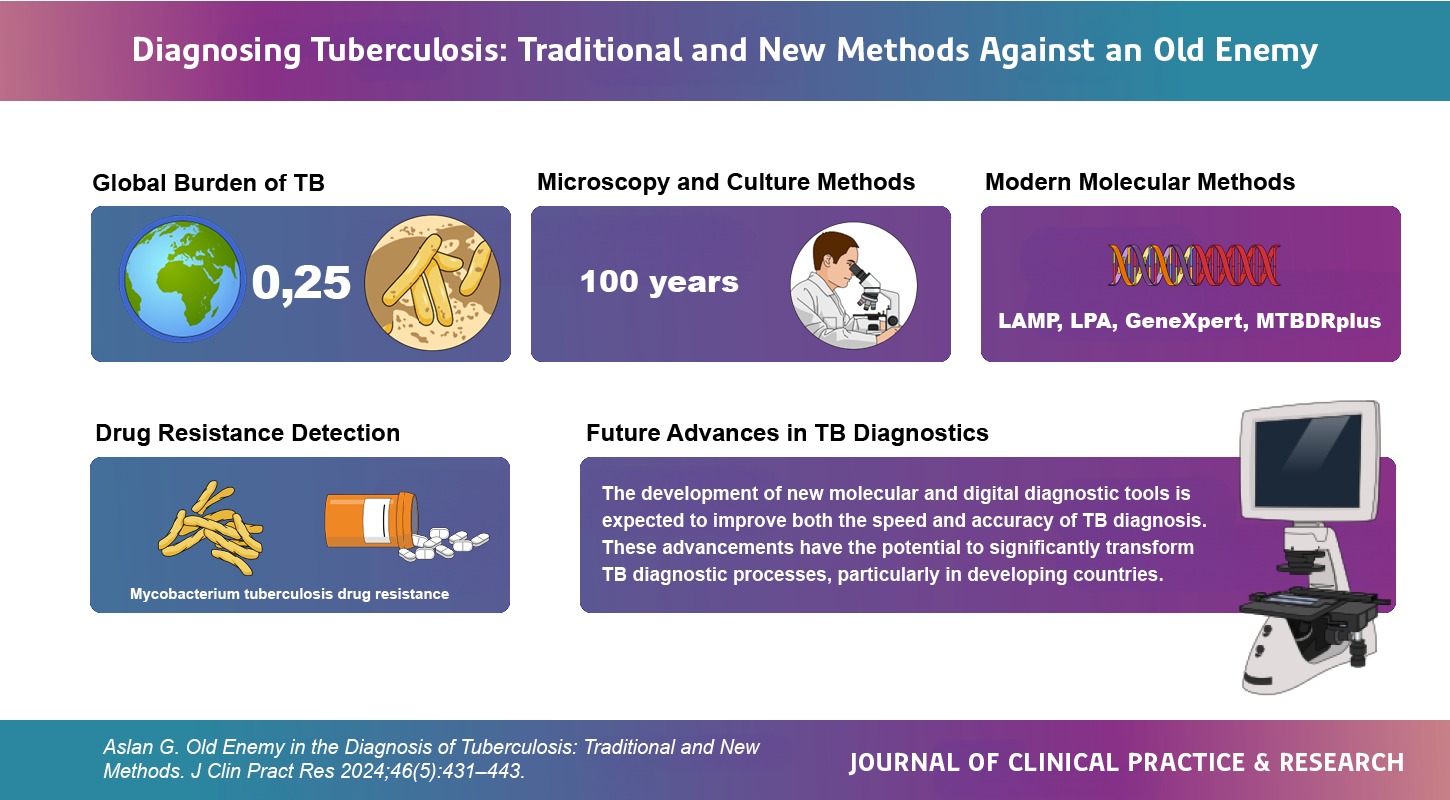
Graphical Abstract